TEMP TO SHARE
FARE's indicator report tracks the growing public health challenge of food allergy in the United States—a top-tier public health issue—highlighting key data that can guide future research efforts.
- Food allergy is a serious immune-mediated disease affecting more than 33 million people in the United States, across all regions and demographic groups, and can cause life-threatening anaphylactic reactions.
- Data shows that the overall burden of food allergy in the U.S. is substantial and growing, with some populations are disproportionately affected.
- Epinephrine remains the only emergency treatment that can stop an anaphylactic reaction.
- Support and funding for food allergy research lags far behind other immune diseases, such as asthma and cancer, despite food allergy affecting more people in the U.S.
- Progress is being made in developing better diagnostic options, innovative therapies, and stronger support systems for patients with food allergy and their caregivers.
- Pursuing a cure will require bold initiative and collaboration across scientific disciplines.
To understand the impact of food allergy in the United States, read FARE’s National Indicator Report on Food Allergy.
Estimated number of people in each state currently living with food allergy.
A Growing Public Health Crisis That Affects Everyone
Food allergy is a serious disease of the immune system that affects more than 33 million individuals in the United States, which is roughly 1 in 13 children and 1 in 10 adults.
Prevalence of convincing food allergy, by allergen type, in a 2015-2016 cross-sectional survey of the U.S. population.
According to the U.S. Food and Drug Administration (FDA), about 90% of food allergies in the United States are triggered by the top nine allergens.
Healthcare providers, families, and food allergy allies need the facts—and FARE has gathered them in one place.
More adults are developing new food allergy later in life. Among the more than 27 million U.S. adults with food allergy, nearly one-half developed at least one food allergy during adulthood, and 21% say that all of their food allergies began after age 18 years.
As this food allergy epidemic grows, so has the frequency of food allergy reactions, which can be life-threatening.
Private insurance claims with diagnoses of food allergy–related anaphylaxis among claims with allergy diagnoses from 2007-2016.
For years, diagnosis has meant that your doctor instructs you to strictly avoid allergen exposure, read every label and know every ingredient, and always carry epinephrine.
Each year, the cumulative cost of food allergy is estimated to be $34.5 billion in 2025 dollars, including $5,928 per child.
Average list price of brand name epinephrine autoinjector, not including manufacturer discounts or rebates.
A New Era
The food allergy community is entering a new era of being empowered and ready to act. Most food allergy patients now have new management options. Emerging therapies can help prevent severe allergic reactions and often allow patients to begin safely consuming small amounts of their allergen.
Looking Forward
The chronic and severe burden of this disease is highlighted throughout FARE’s National Indicator Report for Food Allergy and can only be addressed through an aligned approach in the research, advocacy, clinical, and regulatory sectors.
Every food allergy patient journey is different. But we’re all in this together.
With coordinated action, a world without food allergy is possible. More public health surveys are needed—as well as increased funding for long-term food allergy research, awareness, and education initiatives.
Until then, supportive communities are buit by educating the public and creating allies. Being an ally can be as simple and powerful as understanding that food allergy is a serious disease, respecting food safety needs, and recognizing the signs of a severe allergic reaction and knowing how to give epinephrine.
Did You Know?
Did you know food allergy can affect more than just physical health?
Food allergy doesn’t just affect the body; it affects emotional well-being too. Living with food allergy requires constant vigilance and can create anxiety, depression, and social isolation.
Only 54% of children, 35% of adults, and 27% of caregivers have ever consulted a mental health professional about food allergy–related distress, yet most patients and caregivers report some mental health impacts associated with living with food allergy.
In a study drawing on FARE Patient Registry data, 62% of patients reported mental health concerns related to food allergy.
Food allergy–related mental health concerns among patients with food allergy and their caregivers.
Did you know many people can’t access an allergist?
There are only about 5,200 practicing allergists in the entire United States. That’s roughly 1.6 allergists per 100,000 people. Access is especially limited in rural areas. Only 0.3% of rural counties have an allergist, compared with 23% of urban counties, and only half of allergists accept Medicaid.
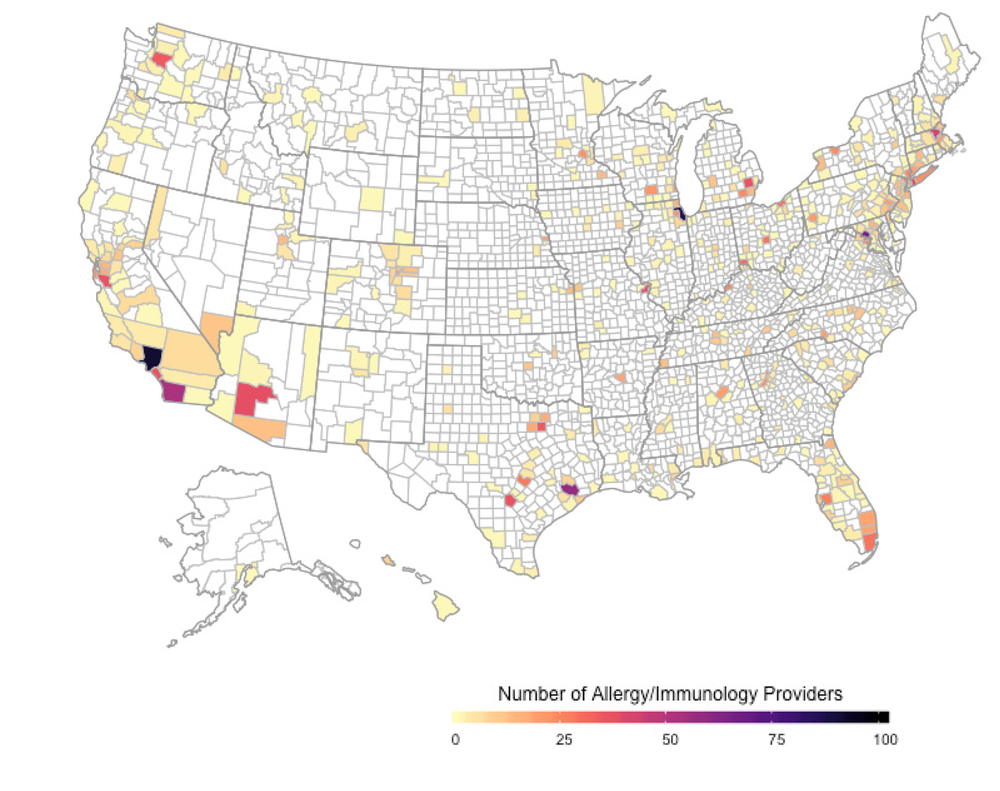
Geographic distribution of allergists at the county level in the United States.
Did you know epinephrine no longer always requires a needle?
Epinephrine is the only medication that can stop a life-threatening allergic reaction. Despite its proven safety and effectiveness, research shows that epinephrine is often under-carried and underused.
In a 2015–2016 cross-sectional survey of individuals with convincing food allergy, only 24% of adults and 40.7% of children reported having a current epinephrine prescription. Notably, in the adult population, those aged 50 years or older were significantly less likely to report having an active epinephrine prescription.
Epinephrine has historically only been available in the form of an auto-injector. In August 2024, the FDA approved a needle-free epinephrine nasal spray, and other delivery systems are being actively tested so patients can have even more options in the future.

Current epinephrine prescription among patients with food allergy, by age, provider diagnosis, and history of food allergy–related emergency department visit.
Did you know that feeding infants commonly allergenic foods (peanuts, eggs, tree nuts, etc.) starting at 4-6 months can help reduce the likelihood of developing a food allergy?
Previous guidance, published in 2000, used to recommend waiting to give infants and toddlers specific allergenic foods, such as peanut and egg. But science has taught us that food allergy rates can be reduced when babies are fed these foods early, often, and in a developmentally appropriate way. A landmark study called the LEAP study showed that introducing peanut-containing foods to infants who already had severe eczema or egg allergy around 4-6 months could reduce their chance of developing peanut allergy by more than 80%.
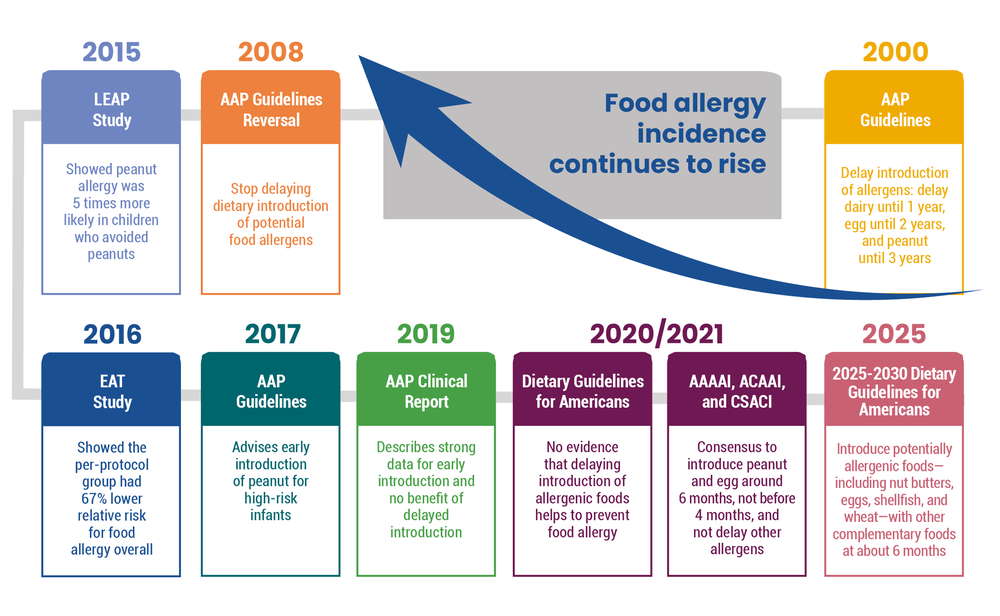
Timeline of “early introduction” guidance and studies for food allergy prevention.
Did you know a tick bite can cause an allergy to meat (and other mammalian products)?
Alpha-gal syndrome is a food allergy to mammalian products that is caused from a tick bite. Between 2017 and 2022, as many as 450,000 people in the U.S. may have developed this allergy. Experts believe the true number is much higher, since many cases go undiagnosed or are never formally reported. Preventing tick bites can prevent this type of food allergy.
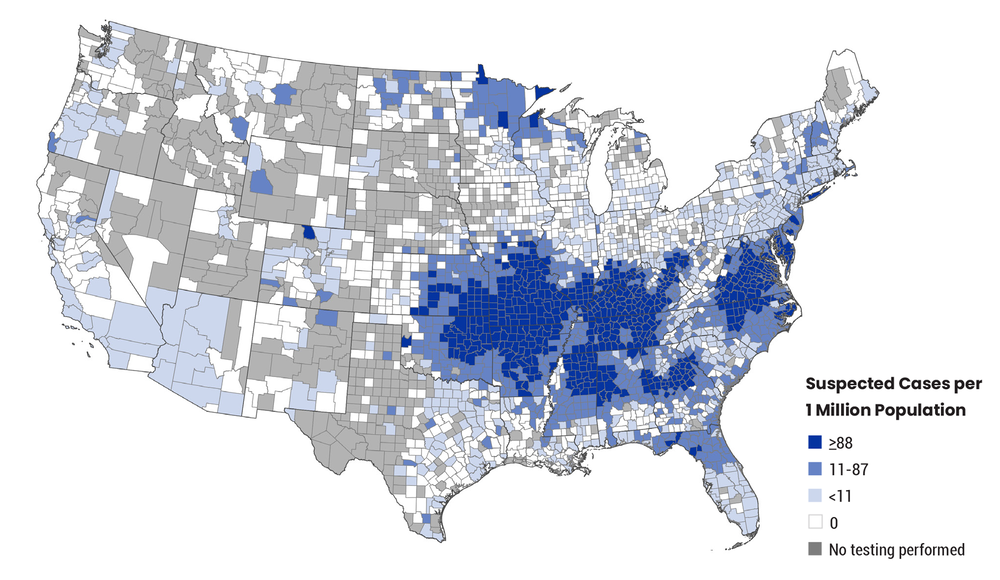
Geographic distribution of suspected alpha-gal syndrome cases from 2017-2022.
Inside the Indicator Report
- 68 pages, 40+ figures and tables, 80+ references
- Prevalence of Food Allergy in the United States
Topics include: Challenges Estimating Food Allergy Prevalence; Estimates of Food Allergy Prevalence; Food Allergy Prevalence by Specific Food Allergen; Multiple Allergies; Adult-Onset Food Allergy - Burden of Food Allergy
Sections include: Food Allergy Reactions; Economic Burden; Psychosocial Burden; Missed School; Allergic Comorbidities; Anaphylaxis and Fatalities - Diagnosis and Management of Food Allergy
Sections include: Access to Specialist Care; Diagnosing Food Allergy; Food Allergic Reaction Management; Therapies for Management of Food Allergy - Food Allergy Prevention
- Selected Food Allergy Syndromes
Sections: Alpha-gal Syndrome; Eosinophilic Esophagitis; Food Protein-Induced Enterocolitis Syndrome; Pollen Food Allergy Syndrome
This indicator report surveys key food allergy science and data, vetted by a diverse team of subject matter experts and thought leaders.
About the Food Allergy AWARE and the Advisory Council
Food Allergy AWARE: Advancing Wellness, Awareness and Resources to Educate is dedicated to increasing awareness and knowledge of the growing prevalence, societal cost, and burden of food allergy as a potentially life-threatening, chronic disease among public health professionals, primary care clinicians, affected patients, caregivers, and the public.
The Food Allergy AWARE Advisory Council (FAAAC) is a diverse team of subject matter experts and thought leaders that represent the voices and perspectives of key stakeholders in food allergy, including primary care clinicians, public health professionals, and those living with or impacted by food allergy. The FAAAC provides guidance and input on surveillance and data collection, indicator report generation, education program development, awareness and promotion plan development/execution, and evaluation and monitoring of overall project reach and impact.
Authorship and drafting of this indicator report were led by Dr. Christopher Warren with extensive input and approval from members of the Food Allergy AWARE Advisory Council.
Members
- Kelly Cleary, MD, FAAP, Medical Director and Vice President of Health and Education for FARE (Food Allergy Research & Education)
- John M. James, MD, President at Food Allergy Consulting and Education Services, LLC (FACES); Chairperson of FAAAC (Food Allergy AWARE Advisory Council), Year 1
- Ashley D. Koranteng, MPH, CHES, Health Engagement Senior Analyst, Cigna
- William A. McCann, MD, MBA, Chief Executive Officer for Allergy Partners
- Jennifer Obenrader, PharmD, CDCES, Clinical Senior Research Project Lead, Research & Analytics, American Medical Group Association (AMGA)
- Michael Pistiner, MD, MMSc, Director of Food Allergy Advocacy, Education and Prevention for MassGeneral Hospital for Children, Food Allergy Center
- Jennifer Platt, DrPH, Director of Research & Programs, Tick-Borne Conditions United
- Sung Poblete, PhD, RN, Chief Executive Officer of FARE (ex officio)
- Rebecca D. Szewczak, DO, FACOFP, ACOFP, Chief Medical Officer at St. Mary’s Regional Medical Center, Enid, Oklahoma
- Christopher M. Warren, PhD, Director of Population Health Research and Research Assistant Professor, Northwestern University Institute for Public Health and Medicine, Department of Preventive Medicine, Division of Epidemiology, Northwestern University Feinberg School of Medicine, Center for Food Allergy and Asthma Research; Chairperson of FAAAC (Food Allergy AWARE Advisory Council), Year 2
- Charisse Wilson, MSHA, Community Health Worker, Food Allergy Parent
- Andrea A. Pappalardo Wlochowicz, MD, Associate Professor of Medicine and Pediatrics, Allergy Service Director, University of Illinois Chicago
This project is supported by the Centers for Disease Control and Prevention of the U.S. Department of Health and Human Services (HHS) as part of a financial assistance award totaling $375,000 with 100 percent funded by CDC/HHS. The contents are those of the author(s) and do not necessarily represent the official views of, nor an endorsement, by CDC/HHS, or the U.S. Government.


